The HESI seizure disorder case study presents a comprehensive exploration of this complex neurological condition, delving into its causes, diagnosis, management, and nursing implications. This in-depth analysis provides valuable insights into the challenges and complexities associated with HESI seizure disorder, offering healthcare professionals and researchers a deeper understanding of this multifaceted condition.
The ensuing paragraphs provide a detailed examination of the various aspects of HESI seizure disorder, shedding light on its prevalence, underlying mechanisms, clinical manifestations, diagnostic criteria, treatment strategies, and the vital role of nurses in patient care. Additionally, the case study offers a nuanced examination of a patient’s journey with HESI seizure disorder, highlighting the challenges and outcomes associated with managing this condition.
Introduction to HESI Seizure Disorder
HESI (Healthcare Excellence through Simulation Innovation) Seizure Disorder is a standardized case study that evaluates nursing students’ knowledge and skills in managing patients with seizure disorders.
Seizure disorders are a group of neurological conditions characterized by recurrent, uncontrolled electrical disturbances in the brain. These disturbances can manifest as a variety of symptoms, including loss of consciousness, convulsions, and sensory or motor impairments.
Prevalence and Impact
Seizure disorders are relatively common, affecting approximately 1% of the population worldwide. They can occur at any age, but are most prevalent in children and the elderly.
Seizure disorders can have a significant impact on individuals’ lives. They can cause physical and cognitive impairments, interfere with daily activities, and lead to social isolation and stigma.
Causes and Risk Factors of HESI Seizure Disorder
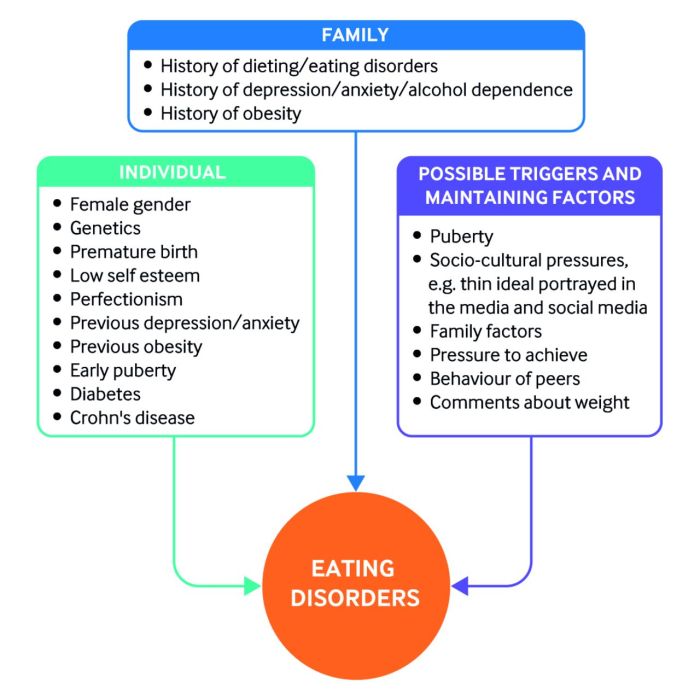
HESI seizure disorder, also known as epilepsy, is a neurological disorder characterized by recurrent, unprovoked seizures. The underlying causes of HESI seizure disorder can be diverse, and identifying the specific cause is crucial for appropriate treatment and management.
Underlying Causes
- Structural Abnormalities:Brain malformations, tumors, or injuries can disrupt normal brain function and lead to seizures.
- Genetic Factors:Certain genetic mutations or syndromes can increase the risk of developing HESI seizure disorder, such as tuberous sclerosis or Down syndrome.
- Metabolic Disturbances:Electrolyte imbalances, hypoglycemia, or hypocalcemia can trigger seizures by altering brain chemistry.
- Infections:Meningitis, encephalitis, or other infections can cause inflammation in the brain and lead to seizures.
- Trauma:Head injuries or other traumatic events can damage brain tissue and increase the risk of seizures.
Risk Factors
Certain factors can increase the likelihood of developing HESI seizure disorder:
- Family History:Having a family member with epilepsy increases the risk of developing the disorder.
- Age:HESI seizure disorder can occur at any age, but it is most common in children and the elderly.
- Neurological Disorders:Individuals with pre-existing neurological conditions, such as autism or cerebral palsy, have a higher risk of developing seizures.
- Alcoholism:Excessive alcohol consumption can increase the risk of seizures, especially in individuals with a family history of epilepsy.
- Sleep Deprivation:Lack of sleep can lower the seizure threshold and trigger seizures in susceptible individuals.
Clinical Presentation and Diagnosis of HESI Seizure Disorder
HESI seizure disorder manifests with a range of clinical features depending on the type of seizure experienced. Generalized seizures involve the entire brain, while focal seizures affect only a specific region.
Clinical Manifestations
- Generalized seizures:Loss of consciousness, tonic-clonic movements (stiffening and jerking), urinary incontinence, tongue biting.
- Focal seizures:Impaired consciousness, focal motor movements (e.g., jerking of one limb), sensory disturbances (e.g., tingling, numbness), psychic symptoms (e.g., hallucinations).
Diagnostic Criteria
The diagnosis of HESI seizure disorder requires:
- History:Description of seizures from the patient or witness.
- Physical examination:Neurological examination to assess for focal neurological deficits.
- Electroencephalography (EEG):Records brain activity and can detect abnormal electrical discharges characteristic of seizures.
Role of Electroencephalography (EEG)
EEG is a non-invasive test that measures brain electrical activity using electrodes placed on the scalp. During a seizure, EEG shows characteristic patterns of abnormal electrical discharges, which can help confirm the diagnosis of HESI seizure disorder and differentiate it from other conditions.
Management and Treatment of HESI Seizure Disorder
The management of HESI seizure disorder involves a combination of pharmacological and non-pharmacological approaches. The primary goal of treatment is to control seizures and prevent their recurrence while minimizing adverse effects.
Anticonvulsant Medications
Anticonvulsant medications are the mainstay of HESI seizure disorder treatment. They work by suppressing the abnormal electrical activity in the brain that causes seizures. Common anticonvulsants used for HESI include:
- Phenytoin
- Carbamazepine
- Valproic acid
- Lamotrigine
- Levetiracetam
The choice of anticonvulsant depends on factors such as seizure type, patient age, and other medical conditions.
Alternative Therapies
In addition to anticonvulsant medications, alternative therapies may be considered for HESI seizure disorder. These include:
- Ketogenic diet:A high-fat, low-carbohydrate diet that has been shown to reduce seizure frequency in some children.
- Vagus nerve stimulation (VNS):A surgical procedure that involves implanting a device that stimulates the vagus nerve to reduce seizure activity.
- Deep brain stimulation (DBS):Another surgical procedure that involves implanting electrodes into the brain to regulate electrical activity.
The efficacy of alternative therapies varies among individuals, and they are typically considered when anticonvulsant medications alone are not effective in controlling seizures.
Case Study of HESI Seizure Disorder: Hesi Seizure Disorder Case Study
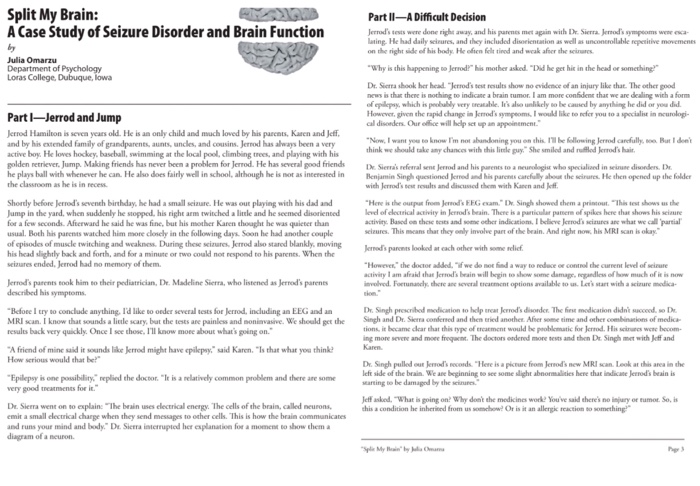
A 25-year-old male presents to the emergency department with a witnessed seizure. The patient’s girlfriend states that he was sitting at home watching television when he suddenly became unresponsive and began to shake. The seizure lasted for approximately 2 minutes, and the patient regained consciousness shortly after it ended.
The patient has no prior history of seizures and has no known risk factors for epilepsy.
The patient’s physical examination is unremarkable, and his neurological examination is normal. An electroencephalogram (EEG) is performed and shows generalized spike-and-wave discharges. The patient is diagnosed with HESI seizure disorder and is started on antiepileptic medication.
Challenges
The management of HESI seizure disorder can be challenging due to the following reasons:
- The diagnosis of HESI seizure disorder can be difficult, as the symptoms can be similar to those of other conditions, such as syncope and psychogenic seizures.
- The treatment of HESI seizure disorder can be challenging, as there is no cure for the condition and the medications used to treat it can have side effects.
- The prognosis for HESI seizure disorder is variable, and some patients may continue to experience seizures despite treatment.
Outcomes, Hesi seizure disorder case study
The outcome of HESI seizure disorder depends on a number of factors, including the severity of the seizures, the patient’s age, and the presence of other medical conditions. With appropriate treatment, most patients with HESI seizure disorder can live normal lives.
Nursing Implications for HESI Seizure Disorder
Nurses play a pivotal role in the care of patients with HESI seizure disorder, providing comprehensive support and ensuring optimal outcomes. Their responsibilities encompass various aspects, including assessment, monitoring, education, and advocacy.
Patient Education and Support
Patient education is crucial in empowering individuals with HESI seizure disorder to manage their condition effectively. Nurses should provide clear and comprehensive information about the disorder, its triggers, medications, and potential side effects. They should also educate patients on seizure recognition and first aid measures, as well as the importance of adherence to medication regimens.
Emotional support is equally essential, as patients with HESI seizure disorder may experience anxiety, fear, and stigma. Nurses should create a supportive and non-judgmental environment, listening attentively to concerns and providing reassurance. They can also connect patients with support groups or other resources to foster a sense of community and belonging.
Advocacy for Patients
Nurses are advocates for patients with HESI seizure disorder, ensuring their rights and needs are met. They can assist patients in accessing appropriate medical care, financial assistance, and educational opportunities. Nurses can also advocate for policy changes that promote equitable access to healthcare and reduce the stigma associated with epilepsy.
Current Research and Future Directions in HESI Seizure Disorder
Ongoing research in HESI seizure disorder focuses on improving diagnosis, understanding the underlying mechanisms, and developing more effective treatments.
Emerging treatment strategies include targeted drug therapies, neuromodulation, and gene therapy. Promising areas for future research include exploring the role of genetics, developing personalized treatment plans, and investigating the potential of non-pharmacological interventions.
Genetic Research
Genetic studies aim to identify genetic mutations and variations associated with HESI seizure disorder. This research can help in early diagnosis, personalized treatment, and genetic counseling.
Question Bank
What is the prevalence of HESI seizure disorder?
HESI seizure disorder is a relatively rare condition, affecting approximately 1 in 100,000 individuals.
What are the most common symptoms of HESI seizure disorder?
The most common symptoms of HESI seizure disorder include seizures, which can range from brief staring spells to full-blown convulsions.
How is HESI seizure disorder diagnosed?
HESI seizure disorder is typically diagnosed based on a combination of patient history, physical examination, and electroencephalography (EEG).
What are the treatment options for HESI seizure disorder?
The primary treatment option for HESI seizure disorder is anticonvulsant medications, which aim to prevent or reduce the frequency and severity of seizures.
What is the prognosis for individuals with HESI seizure disorder?
The prognosis for individuals with HESI seizure disorder varies depending on the severity of their condition and response to treatment. With proper management, many individuals with HESI seizure disorder can live full and active lives.